AI is increasingly being adopted in clinical trials to help teams keep pace with growing data demands. The goal is clear: reduce manual effort, surface insights sooner, and support better decisions. But for many sponsors, those benefits are harder to realize in day-to-day trial work.
Often, the challenge is not the AI itself. It is the infrastructure, including the electronic data capture (EDC) system, underneath it. When the EDC was designed for a different era of clinical research, it can quietly limit how much value AI is able to deliver.
AI Depends on the Foundation Beneath It
AI works best when it has access to timely, well-structured, and connected data. In clinical trials, the EDC system plays a central role in making that possible. It shapes how data is collected, validated, and shared across teams and systems.
When the EDC is flexible and modern, AI can operate continuously and support everyday trial work. When the EDC is rigid or fragmented, AI becomes harder to implement and easier to overlook. This is why many sponsors struggle to translate AI investments into practical improvements.
Where Legacy EDC Systems Create Friction
Legacy EDC platforms were built to meet the needs of earlier studies. While many still handle basic data capture reliably, they often fall short when studies become more complex or data sources expand.
Rigid structures that slow adaptation
Older systems tend to rely on fixed forms and predefined workflows. Making changes mid-study, whether due to protocol amendments or new data requirements, can be time-consuming and disruptive. AI relies on adaptable data structures, and rigid designs make it harder to evolve how data is reviewed or analyzed during an active study.
Limited integration with newer data sources
Many legacy EDC systems were not designed to easily bring in data from wearables, electronic health records, or patient-facing technologies. As these sources become more common, data ends up spread across disconnected tools. AI cannot deliver meaningful insights when it only has access to part of the dataset.
Disconnected workflows and delayed visibility
In older environments, data capture, query management, reporting, and analytics often live in separate systems. This fragmentation slows feedback loops. AI is most effective when it can work with data as it arrives, not days or weeks later.
High effort to introduce change
Legacy platforms often depend on custom development, long release cycles, or external tools to support new capabilities. That makes it harder for teams to test AI-driven approaches or adjust them as study needs evolve.
How These Limitations Reduce AI’s Real-World Impact
When AI is layered onto a legacy EDC, the gaps become apparent quickly.
Insights come too late
If data is only available after scheduled refreshes or batch uploads, AI insights tend to arrive after decisions have already been made. At that point, AI supports reporting rather than active study management.
Manual work persists
Without strong validation rules and integrated data flows, data teams still spend significant time cleaning and reconciling information by hand. AI cannot meaningfully reduce workload if it depends on incomplete or inconsistent inputs.
Confidence in AI suffers
When AI outputs are based on fragmented data, teams may question their reliability. That lack of trust can limit adoption, even when the underlying AI capabilities are sound.
What Modern EDC Platforms Do Differently
Modern EDC systems are designed with flexibility, connectivity, and speed in mind. These characteristics have a direct impact on how effectively AI can be used.
Flexible study design and data models
Modern platforms allow teams to configure and update forms, fields, and workflows without heavy redevelopment. This flexibility supports evolving protocols and creates richer datasets that AI can work with over time.
Built-in interoperability
Support for multiple data sources allows information from sites, patients, and external systems to flow into a single environment. AI can then analyze data across sources instead of in isolation.
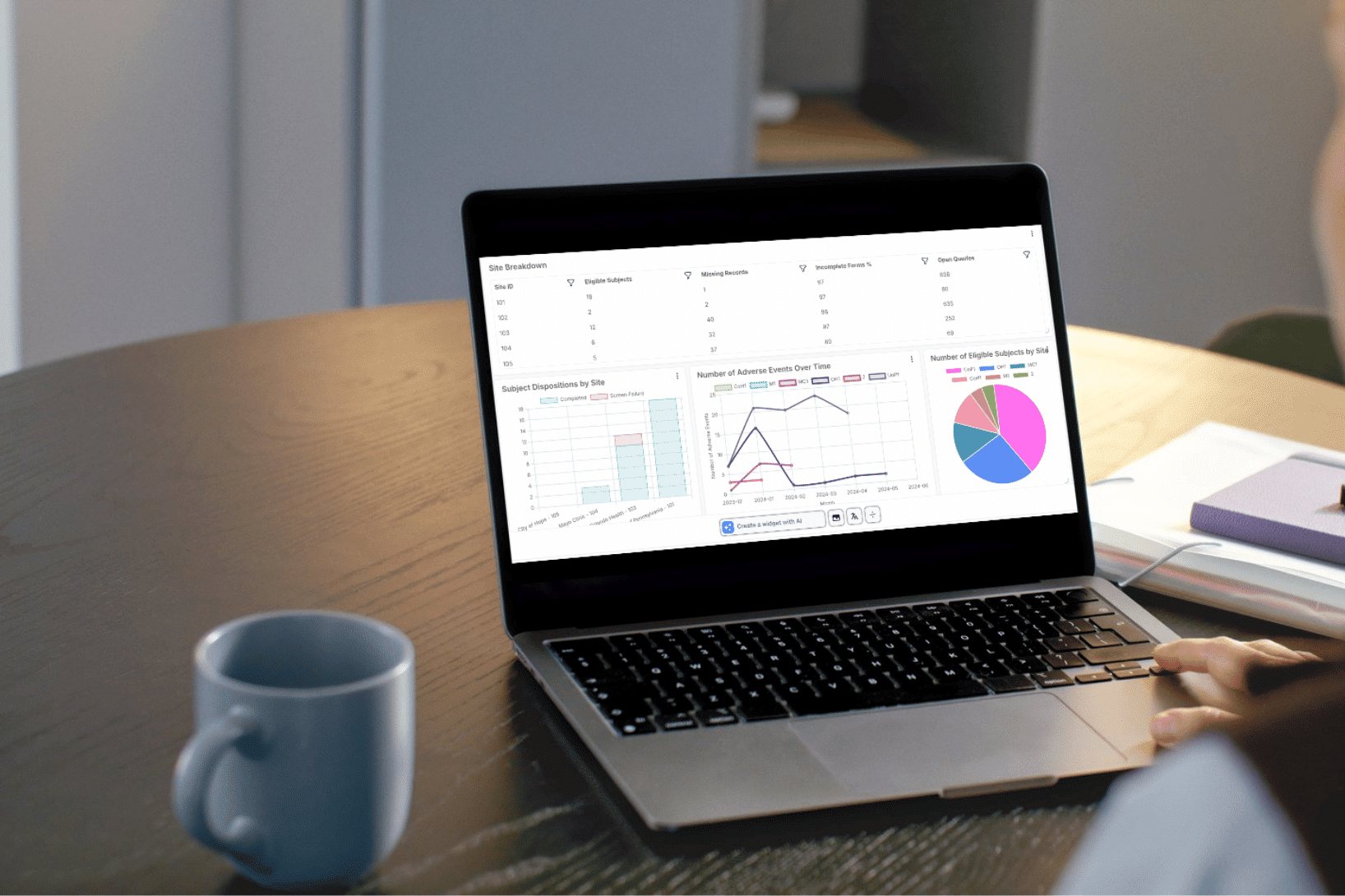
Real-time access to data and analytics
When data is available as it is captured, AI can flag issues, detect trends, and support decisions while there is still time to act. Faster access leads to faster responses and stronger oversight.
Designed for distributed trial models
Mobile-ready data entry helps ensure data is captured promptly and consistently. Faster data flow supports more timely AI-driven insights.
Platforms such as TrialKit reflect this shift toward EDC systems that function as connected data environments rather than static repositories, without requiring teams to rely on disconnected tools.
Reducing Friction When Introducing AI
Even with a modern platform, AI adoption benefits from a practical, measured approach.
Start with data quality
AI amplifies what already exists. Clear data standards, consistent validation rules, and well-defined fields make AI outputs more reliable and easier to trust.
Choose platforms with native analytics
When reporting and visualization are built into the EDC, AI insights are easier to access and understand. Teams are more likely to use AI when it fits naturally into their existing workflows.
Align teams around realistic expectations
AI works best as decision support. Data management, operations, and biostatistics teams should share a clear understanding of what AI can help with and how it fits into daily study work.
Choosing an EDC That Supports AI Impact
AI will continue to evolve, but its impact will always depend on the systems that support it. As studies become more complex and data sources expand, EDC platforms that cannot adapt risk holding teams back.
Sponsors looking to get real value from AI should take a close look at whether their current EDC supports flexibility, integration, and real-time access. When the EDC is built to support modern data workflows, AI becomes easier to implement and more likely to deliver meaningful results.
The takeaway is straightforward: AI can improve clinical trial data management, but only when the underlying platform allows it to be part of everyday execution.
For more information about how TrialKit can help you unlock the benefits of AI in your clinical trial data, visit us today.